By Jennifer Collins, Vizient
“After looking at Vizient’s Clinical Team Insights data, organizations need to prepare for these changes because it could significantly impact organization’s ability to meet patient demands while maintaining viability in the market.” — Christen Hunt, DNP, NP-C, CPNP-AC Vizient Senior Director, Clinical Team Insights
To say the healthcare industry has faced multiple challenges over the last few years would be an understatement. Healthcare organizations continue to address various clinical workforce issues, which can result in inadequate time available to prepare for important billing changes provided in the 2022 Medicare Physician Fee Schedule Final Rule . While the 2023 Physician Fee Schedule proposed rule should be released in the coming weeks, it is important to be aware of the anticipated impact of the agency's previously finalized policy, especially if the Centers for Medicare and Medicaid Services (CMS) considers revisions in the upcoming proposed rule.
Notably, the 2022 final rule provided changes to determine which provider should bill when performing a split/shared evaluation/management (E/M) visit for both 2022 and 2023. For 2022, CMS provided a transitional year where billing the substantive portion could be based on either a key component (this could have included the history, exam or medical decision making) or based on time. By 2023, this policy would change so that the substantive portion must be based on time. Therefore, based on the 2022 final rule, to bill a split/shared visit, the billing provider must perform more than half of the total time, starting January 1, 2023.
"While hospitals and other healthcare providers have endured drastic changes during the pandemic and workforce shortages, this seemingly minor shift in policy is important to understand as it may impact how advanced practice practitioners (APPs) and physicians deliver care, among other implications," says Christen Hunt, DNP, NP-C, CPNP-AC, senior director, clinical team insights. "After looking at Vizient's Clinical Team Insights data, organizations need to prepare for these changes because it could significantly impact organizations' ability to meet patient demands while maintaining viability in the market."
The current state of our care teams
Leveraging data from Vizient's Clinical Team Insights 2020 data brief, the average physician to APP ratio is 2:1. Still, we see a wide variation in this ratio ranging from one physician per APP to 5.2 physicians per APP. In addition to the physician to APP ratio, it is also important to note that 67% of hospitalist teams include APPs, and 40% of intensivists teams include APPs.
Hunt notes that over the last few years, we have seen a rapid increase in the employment of APPs on the inpatient care delivery team in response to the physician shortage. "Consequently, by leveraging all care team members' expertise, improved quality outcomes have been achieved but organizational structures and processes have not evolved to fully support the care team, leaving significant variations in roles and responsibilities," says Hunt.
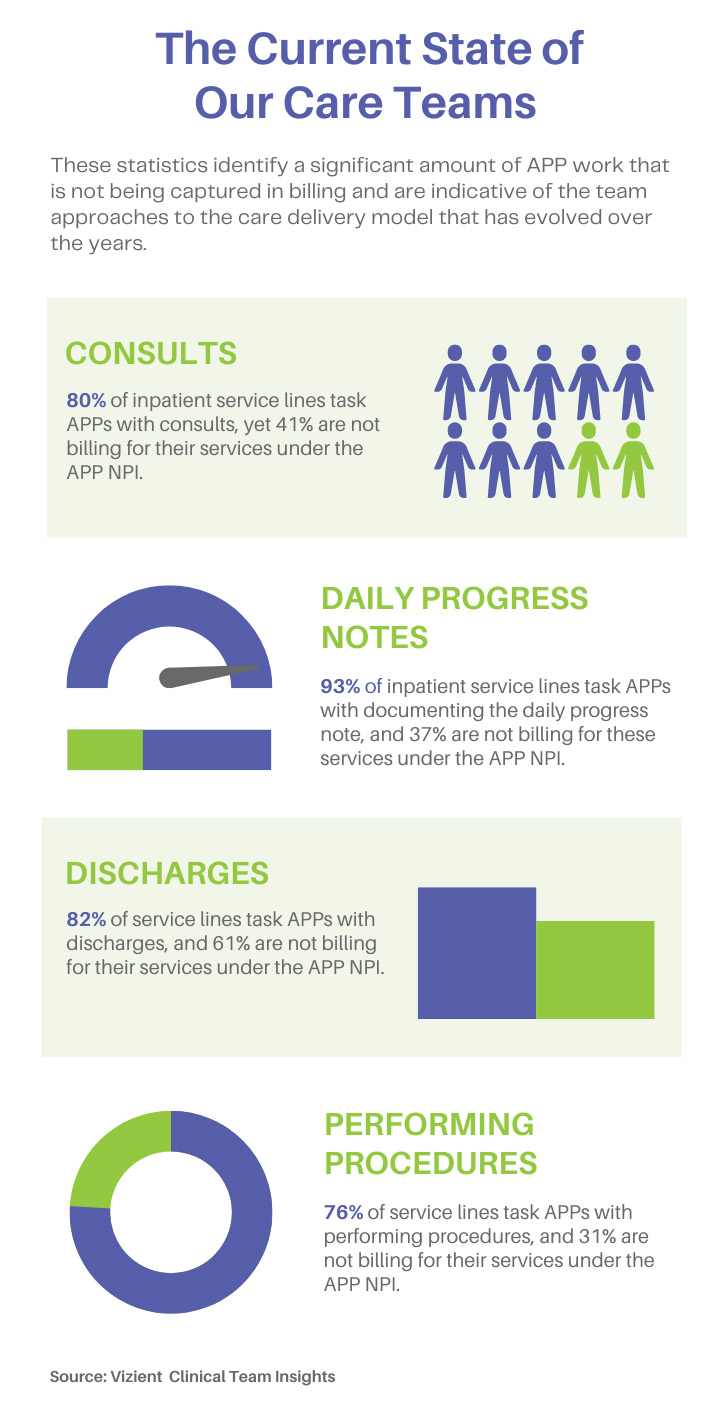
The Clinical Team Insights data identified some of the variations in the roles and responsibilities of APPs (see sidebar). This led to a review of organizational structures and processes such as compensation models and productivity measures. Of the physicians compensated for productivity, 36% receive credit for APPs' work relative value unit (wRVU). Only 30% of hospitals are tracking APP inpatient productivity, with only 7% including billed visits as a measurement of productivity with nearly 100% of physician productivity based on a component of wRVUs.
"These statistics identify a significant amount of APP work that is not being captured and describe the team approaches to the care delivery model that has evolved over the years. Just as we find the significant variation in roles and responsibilities, we find that compensation models and productivity measurements did not evolve leaving many organizations accepting not fully understanding the individual productivity of the APPs," notes Hunt.
Predicted impact on healthcare organizations
It's important to ensure your organization is prepared to alleviate potential disruption and division within care teams. While the 2023 physician fee schedule proposed rule may address split/shared visits in some way, organizations should be aware of the current policy landscape and start to prepare.
"As the supply of physicians cannot meet the current demands of patients without their APP colleagues and the integrated care team model that has evolved, the agency's interest to change split/shared E/M visits in conjunction with the current care model may ultimately result in more APPs billing for E/M services to maintain compliance," says Hunt. This will result in 85% reimbursement instead of the 100% physician fee schedule which was provided when the physician billed for the split/shared E/M visit previously. Hunt notes that the 15% decrease in reimbursement threatens many organizations as they are already struggling financially with various workforce challenges, including increased labor costs.
Maintaining the current care delivery model while becoming compliant with the billing changes could also significantly impact physicians' income and measurement of productivity. If the APP performs 50% of the total time with the patient and becomes the billing provider, this will indirectly impact the physicians' salary and incentive pay based on individual production/revenue. "If compensation methodology doesn't change, there is concern the Medicare changes may undermine team-based care and encourage physicians to limit their collaboration with APPs to maintain wRVUs/ revenue production thus impacting access," says Hunt
How to prepare for the changes
Assuming the 2023 physician fee schedule rule does not provide substantial modifications to the split/shared E/M visit policy, preparing appropriately is critical, especially if no changes have been made during this transitional year. Hunt recommends that organizations first examine their current care delivery models to understand how providers spend their time with patients. "Specific tasks to assess include chart review, documentation of the visit, face-to-face care provided, procedures and coordination of care," says Hunt. You'll next want to understand who is billing for the services and where split/shared E/M visits are being billed. "A clear understanding of the current state of how the care teams are operating, billing for their services and organizational processes such as compensation methodology and measurements of provider productivity will display the potential impact on your organization," notes Hunt.
Once the current state assessment is complete, you can start building your organizational structures and processes to meet the organizational strategic goals. Hunt notes that this may require changing the way productivity is measured and provider compensation. "Suppose the clinical workforce can meet the organization's strategic goals by functioning as a team. In that case, team metrics may motivate the team to work together, focusing on the needs of the patient population leveraging the entire team expertise," says Hunt. This step is complex, requiring new and innovative compensation models and metrics to measure productivity. "Care teams know how to work together efficiently, but it is now time for the organizational structure to support our clinical care teams."
As hospitals continue to address clinical workforce issues, it's important to know how the 2022 final rule impacts you so that you can be better informed. To learn more about preparing your organization for the future, please contact Vizient Clinical Team Insights to help or our Office of Public Policy and Government Relations for policy-related questions or concerns.