As blockbuster biologics continue to come off patents, biosimilars are poised to play a crucial role in reshaping the treatment landscape for cancer and other chronic conditions. Besides producing equivalent outcomes to their biologic reference products, biosimilars are also expected to help lower the overall cost of health care.
These industry forces create new opportunities for health systems to adopt biosimilar policies and champion their inclusion on formularies. To determine which biosimilars are appropriate for inclusion, leaders will need to carefully evaluate the savings opportunities with each product.
Shifting reimbursement policies
A 2018 report estimated that biosimilars would represent a total future savings potential of $54 billion between 2017 and 2026. However, realizing this savings potential will require biosimilar adoption at a faster pace than we’ve seen. A major barrier to uptake is reimbursement. Policy changes are beginning to resolve disparities in Medicare reimbursement between biosimilars and originator, branded biologics, but there are still financial hurdles to clear. Many commercial payers dictate a preferred originator product or a biosimilar product and require additional prior authorization steps for reimbursement of non-preferred formulary product, creating additional administrative burden for providers. In some instances a payer may only cover a biosimilar if the patient “fails” on a branded product first, which creates an additional challenge for health systems having to fully convert to a specific biosimilar.
“Though biosimilars are expected to be priced 15 to 30% below that of their reference products, reimbursement policies for biosimilar therapies do not always translate to overall, improved post-reimbursement value,” said Mittal Sutaria, vice president, pharmacy contracting and program services for Vizient. “Ultimately, health systems need to keep abreast of changing reimbursement policies by each payer for biosimilars in order to provide the highest quality, lowest cost care that maximizes value for patients,” said Sutaria.
Helping members crunch the numbers
When assessing the savings potential of biosimilars relative to their reference product, health systems must examine multiple components: the upfront acquisition cost of each product, potential conversion opportunities, and coverage and reimbursement rates from payers.
Vizient recently launched a financial evaluation tool to help pharmacy program members with the assessment process. Developed with member input, the calculator helps members assess biosimilars against associated reference biologics to understand the savings opportunities and margin improvement across multiple products.
The tool contains all biosimilar and reference products on the market and is updated as new biosimilars become available. This analytic tool allows members to test different product scenarios, whether it is converting to one biosimilar or having a mix of products. Flexible and personalized to meet member needs, the tool illustrates the financial impact of biosimilar formulary decisions.
Let’s say a hypothetical health system wanted to compare originator product Rituxan to its biosimilars, Truxima and Ruxience. Pharmacists and finance team members would work together to input information for all three products into the tool including:
- Product acquisition price
- Historical annual usage
- Anticipated conversion to each biosimilar
- Payers and payer mix
- Product reimbursement rates by payer
- Additional rebates or discounts
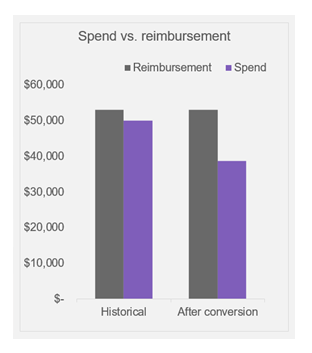
After a user provides these inputs, the tool calculates net margin for each product, along with potential reimbursement, spend and margin as a result of the conversion to a biosimilar.
Understanding the financial impact of product decisions
Health systems are challenged with properly evaluating biosimilar products from a financial, clinical and operational standpoint to ensure that the most cost effective therapies are used. When analyzing the overall financial impact of a biosimilar on a health system, many variables must be evaluated.
“The provider setting in which the drug is administered has implications, since acquisition costs and reimbursement models vary depending on sites of care,” Sutaria noted. “With an increasing number of biosimilars in the pipeline that are used in the outpatient setting, reimbursement becomes a greater financial focus in the cost savings equation. Additionally, the procurement costs may vary based on total purchase volume or market share commitment for a specific product.”
Further, as the market has matured, multiple biosimilars are often available for the same reference product. Each product may have different reimbursement rates, making the evaluation process even more complex.
The era of biosimilars is here
In the coming months, several competing biosimilar versions of blockbuster biologics are expected to reach the market, including Rituxan (rituximab), Avastin (bevacizumab) and additional Herceptin (trastuzumab) biosimilars. These new entrants, along with existing biosimilars, offer expanded therapeutic options for patients while lowering drug costs.
“The time is right for health systems to establish a biosimilars strategy,” said Sutaria. “To do this, organizations must understand the market dynamics that influence the uptake of biosimilars, including pricing strategies, managed care influences and regulatory policies.” This information will assist leaders in assessing the value of a biosimilar compared to its reference product in terms of price, reimbursement and developing strategies for appropriate biosimilar use across the health system.
Vizient offers pharmacy program members comprehensive evidence-based clinical resources to support them in their formulary evaluations of approved and pending biosimilars. For more information about the Vizient pharmacy program or the biosimilars financial evaluation tool, contact us today.