by Nancy Masaschi and Kristi Biltz
Clinical Advisory Solutions
This blog post is part one of a five-part series on clinical-supply integration, a process for informed business decisions that engage clinicians, preserve quality and safety and lead to greater patient satisfaction. Read the other blogs in this series:
- Getting from Good to Great: Using Data to Move From Traditional Product Standardization to Clinical-Supply Integration
- Moving from Value Analysis to a Clinical-Supply Integration Model: Engagement and Alignment are Key
- How Do You Know What You Know? 3 Ways Clinical-Supply Integration Can Help You Make Better Decisions
- Clinical-Supply Integration vs. Value Analysis: Is There a Difference?
Clinical-supply integration (CSI) has become a recognizable concept for many health care organizations as they continue to focus on performance improvement. But many are unsure how to operationalize a CSI model that fits their organization.
At a high level, CSI seeks to further integrate the clinical staff into decision-making. Within the model, there are four domains: engagement, insights, knowledge and process. The domains are integral to bringing a CSI model to fruition.
In this blog post, we’ll concentrate on the process domain of the CSI model. Specifically, we’ll share guidance on moving to a CSI model from a traditional value analysis (VA) model.
Process is establishing a system-wide change management discipline that implements decisions and drives continuous improvements throughout the health care continuum. A systematic approach to change management aligns processes and is the essence of how the CSI model is delivered.
Three areas within the process domain that are foundational to how CSI is realized are a clinical scorecard, clinical variation reduction, and ownership and accountability.
1. Traditional value analysis savings tracker versus a CSI clinical scorecard
The way in which a program measures success covers four key areas: goals, driver of goals, reporting and metrics. We have broken these areas down and highlighted key differences between value analysis and CSI.
|
New Product Request (NPR) versus Clinical Variation Reduction |
||
|
Attribute |
Traditional Value Analysis |
Clinical Supply Integration |
|
Approach |
Reactive to wants |
Proactive to outcomes |
|
Results |
Increase in supply and clinical variation |
Decrease in supply and clinical variation |
|
Customer |
Physician as customer |
Patient as customer |
|
Focus |
Product only |
Product and clinical practice |
Goals
When we think of a traditional value analysis savings tracker, we usually think of tracking non-labor expense-related cost savings with the single goal of decreasing the annual budget. The goals of CSI are to reduce costs across the continuum of care as well as improve patient outcomes and quality measures.
Driver of goals
Savings goals are typically driven by supply chain in traditional value analysis, focusing mainly on savings through product negotiation or product standardization. CSI expands the focus to include quality and outcomes. Without focusing on cost, quality and outcomes equally, successfully engaging physicians is difficult. The clinician-led process in CSI engenders stronger engagement and a commitment to generating savings and improving quality and outcomes. This ultimately leads to a substantial impact on overall organizational performance.
Reporting approaches
How do you shift from a supply chain-led endeavor to one where physicians own and drive the process? Traditionally, the data shows spend and cost with retrospective cost-benefit analyses focusing on supplier market share and compliance. The transition to the CSI process introduces physician-level data such as outcomes, quality, usage, and revenue impact into the review process. This data highlights cost reduction and quality improvement opportunities.
Metrics
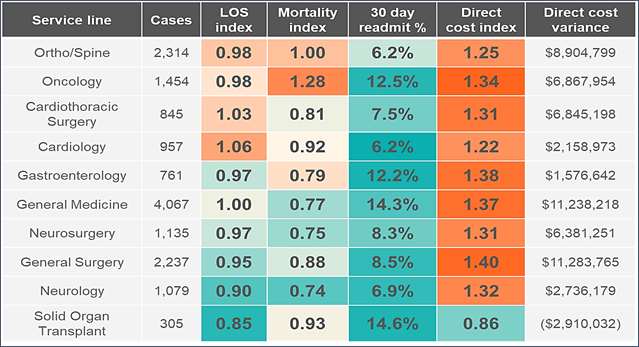
Savings trackers typically consist of initiatives, each with a single savings target based on a cost-benefit analysis. When you migrate to CSI, you’re incorporating the impact that this initiative could bring to the total cost of care into a dashboard. (See table below.) It pulls in various key metrics that tell the story around that initiative and the impact it has not only on cost, but also on quality and outcomes.
2. New product request versus clinical variation reduction
VA teams often struggle to balance new product requests with the need to work on strategic imperatives. As hospitals strive to improve patient outcomes, the CSI model is better able to meet these new expectations. Here are four strategies to help you shift the emphasis from product requests to clinical variation reduction in a CSI model.
|
New Product Request (NPR) versus Clinical Variation Reduction |
||
|
Attribute |
Traditional Value Analysis |
Clinical Supply Integration |
|
Approach |
Reactive to wants |
Proactive to outcomes |
|
Results |
Increase in supply and clinical variation |
Decrease in supply and clinical variation |
|
Customer |
Physician as customer |
Patient as customer |
|
Focus |
Product only |
Product and clinical practice |
Approach
When the majority of requests are for new products, the focus is on reacting to the clinicians’ wants instead of taking proactive steps to impact clinical outcomes. Encouraging quality indicators that focus on outcomes will move you toward the proactive approach to product acquisition. Physicians are more likely to come to the table when you show them how they’re performing compared to their peers.
Results
When taking a reactive approach, approving requests generates additional SKUs. The result is an increased variation in clinical practice. Focus on decreasing variation at both the SKU and practice levels through a physician comparative analysis that relies heavily on peer discussion. This effort will reduce both practice and product variation.
Customer
In traditional value analysis, the physician is thought to be the customer and their requests are often granted with little vetting. CSI models start by identifying a process or practice variation that may or may not involve products. Instead, the starting point is often quality data or contracts. In CSI, the focus shifts from buying products to buying outcomes.
Focus
In value analysis, products are reviewed in isolation with cost analytics as the driver. In CSI, the analysis incorporates not only the requested product, but all the products used for a particular diagnosis related group or procedure and how those products are used in clinical practice.
3. Roles and responsibilities versus owner and accountability
Outlining roles and responsibilities is important to any process. However, in CSI, ownership and accountability are also critical to success.
|
Roles and Responsibilities versus Owner and Accountability |
||
|
Attribute |
Traditional Value Analysis |
Clinical Supply Integration |
|
Physician role |
Physician stakeholder role |
Physician leader/owner |
|
Structure |
Multi-disciplinary |
Service line |
|
Scope |
Broad scope |
Targeted scope |
Physician Role
In VA, physicians are considered participants. Usually those physicians are provided with the opportunities and strategy from supply chain. Advancing to a model where physician leaders own the goals, drive the initiatives, and are accountable for their strategies toward improved quality outcomes will advance your program.
Structure
In the traditional value analysis model, multidisciplinary teams with individuals from many departments are brought together to review a wide variety of opportunities. In CSI, the opportunities are directed toward specific service lines while maintaining input from safety, infection control, biomedical engineering, and risk. A service line structure enables focused clinical groups to have productive conversations and to align around common goals.
Scope
Under VA, opportunities such as trauma may address a wide topic around a particular product category. With CSI, the opportunities are specific with a targeted scope and goal. The opportunity may be to look at the clinical practice patterns of a particular procedure or the utilization of certain devices or technology and weigh that into a particular clinical outcome.
Of the four CSI domains, process operationalizes the model to deliver change and improve organizational performance. Process links engagement, insights and knowledge and allows for an improvement strategy focused on reducing costs and improving quality and outcomes. Developing a systematic process for change management will accelerate your journey to clinical-supply integration.
Clinical-supply integration is an ongoing, interdisciplinary strategy encompassing four performance domains — engagement, insights, process and knowledge — to inform decision making about products and services in order to eliminate harm, improve outcomes and lower costs. Read about the domains in the related articles below or learn more about clinical-supply integration.
About the authors